Find Out How To Treat Bursitis Of The Foot?
Retrocalcaneal bursitis is closely related to Haglund?s Deformity (or ?pump bumps?). If you have a bony enlargement on the back of the heel that rubs the Achilles tendon, it can cause the formation of a bursa (small fluid filled sack). It usually happens in athletes as shoes rub against the heel. The bursa can aggravated by the stitching of a heel counter in the shoe as well. It can make wearing shoes and exercising difficult. Another term used for this condition is ?pump bump? because it can frequently occur with wearing high heels as well. ?Retro-" means behind and ?calcaneus? means heel bone. So this is precisely where the bursitis (inflammation of the bursa) develops. Once it begins and you develop bursitis between the heel bone and the Achilles tendon, it can become even more painful. When most people first notice retrocalcaneal bursitis, it is because the skin, bursa and other soft tissues at the back of the heel gets irritated as the knot of bone rubs against the heel counter in shoes. The back of the shoes create friction and pressure that aggravate the bony enlargement and pinches the bursa while you walk.
Causes
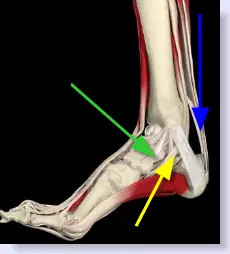
Pain at the posterior heel or ankle is most commonly caused by pathology at either the posterior calcaneus (at the calcaneal insertion site of the Achilles tendon) or at its associated bursae. Two bursae are located just superior to the insertion of the Achilles (calcaneal) tendon. Anterior or deep to the tendon is the retrocalcaneal (subtendinous) bursa, which is located between the Achilles tendon and the calcaneus. Posterior or superficial to the Achilles tendon is the subcutaneous calcaneal bursa, also called the Achilles bursa. This bursa is located between the skin and posterior aspect of the distal Achilles tendon. Inflammation of either or both of these bursa can cause pain at the posterior heel and ankle region.
Symptoms
Your heel may feel more sensitive to the cold and ache in cold and damp weather due to impaired circulation. These symptoms are often the result of failure to treat the injury properly from the outset and overicing.
Diagnosis
A physical examination will be performed to determine if you have any signs of Achilles Bursitis or other ankle injury. He/she will look and feel the soft tissue and bones in your ankles to note any differences between the two of them. This will identify any abnormalities, such as swelling, bone deformities, atrophied muscles, redness and/or warmth on the skin. In many cases, the first sign that you have Achilles bursitis is swelling in the back of the foot and ankle pain.
Non Surgical Treatment
So what can you do to alleviate this type of pain in the foot? If the bursitis pain is occurring on the toes, bunion or back of the heel area the smart money would be on eliminating the shoes that seem to aggravate the condition. Eliminating these shoes may not in itself clear up the problem but you can be sure that if you continue to wear the offending shoes nothing you or your doctor do will permanently ?fix? the problem. A recurring theme that I use throughout this site that if you put an abnormally shaped foot in a dressy shoe it is literally the same as trying to put a square peg in a round hole, it will not fit. OK, so you threw away those dressy shoes and the foot still hurts, now what? Depending on the severity of the pain, over the counter anti-inflammatory medication may do the trick. The key here is to take the medication on an ongoing basis, according to the directions on the package to build up therapeutic blood levels. Assuming you can tolerate this type of medication, along with alternative treatments you can try). take the medication for 10-14 days. Stop if the symptoms have not dramatically improved. Icing the area during this period may also help reduce the symptoms.
Prevention
Contact your physician if bursitis pain is disabling (when movement of the joint is largely or entirely restricted), if the pain doesn?t subside after a week of self-care, or if the joint is red and swollen. Also call your doctor if you develop a fever, which could signal infectious bursitis-a condition that especially can afflict the elbow. Except for the fever, symptoms resemble other forms of bursitis, but infectious bursitis requires immediate medical attention.
Hammer Toe Decreasing Surgery
 Overview
Overview
A Hammer toes occurs when the joint of the toes curl down. The reason they curl abnormally is due to a muscle imbalance which results in the tendons becoming unnaturally tight. They are due to Heredity, improper shoes, and Arthritis. There are two types of hammer toes, flexible or rigid. These classification are based on the mobility of the toe joints. A flexible hammer toe is one with a flexible toe joint that allows it to be straightend with your finger. In time a flexible joint may turn into a rigid hammer toe. Normally flexible hammer toes are much less painful than rigid hammer toes. A rigid hammer toe is one with a rigid toe joint, one that is not moveable with your finger. These rigid toe joints can be very painful and limit the ability to move.
Causes
Hammertoe has three main culprits: tight shoes, trauma, and nerve injuries or disorders. When toes are crowded in shoes that are too tight and narrow, they are unable to rest flat, and this curled toe position may become permanent even when you aren't wearing shoes due to the tendons of the toe permanently tightening. When the tendons are held in one position for too long, the muscles tighten and eventually become unable to stretch back out. A similar situation may result when tendons are injured due to trauma, such as a stubbed, jammed, or broken toe.
 Symptoms
Symptoms
Hammertoe and mallet toe feature an abnormal bend in the joints of one or more of your toes. Moving the affected toe may be difficult or painful. Corns and calluses can result from the toe rubbing against the inside of your shoes. See your doctor if you have persistent foot pain that affects your ability to walk properly.
Diagnosis
Hammer toes may be easily detected through observation. The malformation of the person's toes begin as mild distortions, yet may worsen over time - especially if the factors causing the hammer toes are not eased or removed. If the condition is paid attention to early enough, the person's toes may not be permanently damaged and may be treated without having to receive surgical intervention. If the person's toes remain untreated for too long, however the muscles within the toes might stiffen even more and will require invasive procedures to correct the deformity.
Non Surgical Treatment
If your hammertoe problem is diagnosed as flexible hammertoe, there are a number of nonsurgical treatments that may be able to straighten out your toe or toes and return them to their proper alignment. Padding and Taping. Your physician may pad the boney top-part of your hammertoe as Hammer toe a means of relieving pain, and may tape your toes as a way to change their position, correct the muscle imbalance and relieve the pressure that led to the hammertoe's development. Medication. Anti-inflammatory drugs such as aspirin and ibuprofen can help deal with inflammation, swelling and pain caused by your hammertoe. Cortisone injections may be prescribed for the same purpose. If your hammertoe is a consequence of arthritis, your physician may prescribe medications for that.
Surgical Treatment
If conservative measures fail to provide relief, or if your hammertoe is in advanced stages with rigidity and a significant amount of pain, surgery may be required. Some patients also require surgery if they have open sores or wounds related to their hammertoe. For patients who also suffer from bunions, a combined procedure may be appropriate, addressing both conditions within the same surgery. Recovery time will vary from patient to patient, depending on the extent of the surgical repair and other conditions that may also be present.
Hammer Toes Causes And Cures
 Overview
Overview
hammertoe, also called hammer toe, deformity of the second, third, or fourth toe in which the toe is bent downward at the middle joint (the proximal interphalangeal [PIP] joint), such that the overall shape of the toe resembles a hammer. Most cases of hammertoe involve the second toe, and often only one or two toes are affected. In rare cases when all the toes are involved, a thorough neurological assessment is necessary to evaluate for underlying nerve or spinal cord problems.
Causes
Footwear can contribute significantly to the development of hammertoes. Shoes that are too small force your toes into a curled position. Over time, your toe tendons adjust to this positioning, causing your toe or toes to hold a hammered shape. Athletes may be especially susceptible, because of the increased forces on the toes from shoes that are too small or tight. Heel elevation in footwear is also problematic, as it causes your toes to be pushed into the shoe?s toe box. Heel elevation additionally contributes to muscle imbalance. A common example of this is when your Achilles tendon-the tendon at the back of your leg that attaches your calf muscles to your heel bone-is too tight, causing the tendons on the top of your foot that attach to your toes to work too hard and hold your toes in an unnatural, elevated position.
 Symptoms
Symptoms
Hammer toe is often distinguished by a toe stuck in an upside-down ?V? position, and common symptoms include corns on the top of your toe joint. Pain at the top of a bent toe when you put on your shoes. Pain when moving a toe joint. Pain on the ball of your foot under the bent toe. Corns developing on the top of the toe joint. It is advisable to seek medical advice if your feet hurt on a regular basis. It is imperative to act fast and seek the care of a podiatrist or foot surgeon. By acting quickly, you can prevent your problem from getting worse.
Diagnosis
First push up on the bottom of the metatarsal head associated with the affected toe and see if the toe straightens out. If it does, then an orthotic could correct the problem, usually with a metatarsal pad. If the toe does not straighten out when the metatarsal head is pushed up, then that indicates that contracture in the capsule and ligaments (capsule contracts because the joint was in the wrong position for too long) of the MTP joint has set in and surgery is required. Orthotics are generally required post-surgically.
Non Surgical Treatment
There is a variety of treatment options for hammertoe. The treatment your foot and ankle surgeon selects will depend upon the severity of your hammertoe and other factors. A number of non-surgical measures can be undertaken. Padding corns and calluses. Your foot and ankle surgeon can provide or prescribe pads designed to shield corns from irritation. If you want to try over-the-counter pads, avoid the medicated types. Medicated pads are generally not recommended because they may contain a small amount of acid that can be harmful. Consult your surgeon about this option. Changes in shoewear. Avoid shoes with pointed toes, shoes that are too short, or shoes with high heels, conditions that can force your toe against the front of the shoe. Instead, choose comfortable shoes with a deep, roomy toe box and heels no higher than two inches. Orthotic devices. A custom orthotic device placed in your shoe may help control the muscle/tendon imbalance. Injection therapy. Corticosteroid injections are sometimes used to ease pain and inflammation caused by hammertoe. Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation. Splinting/strapping. Splints or small straps may be applied by the surgeon to realign the bent toe.
Surgical Treatment
Surgery is the approach that is often necessary to correct hammertoe that fails to respond to nonsurgical management. Surgery is appropriate when the muscles and tendons involved in a hammertoe problem have become so tight that the joints are rigid, misaligned and unmovable. There are a number of surgical techniques for dealing with the complex range of joint, bone, muscle, tendon and ligament abnormalities that define each hammertoe's make-up. To correct a hammertoe deformity, the Hammer toe surgeon's goal is to restore the normal alignment of the toe joint, relieving the pressure that led to the hammertoe's development (this should also relieve the pain, as well). To do this, he or she may remove part of the boney structure that creates a prominence at the top of the joint. Tighten or loosen the muscles, tendons and ligaments around the toe joints. Realign the toe bones by cutting one or more and shifting their position, realigning muscles, tendons and ligaments accordingly. Use screws, wires or plates to hold the joint surfaces together until they heal. Reconstruct a badly damaged joint or replace it with an artificial implant.
Foot Bunions Prevention
Overview
 A bunion is an often painful enlargement of bone or tissue around the joint at the base of the big toe. If you have a bunion, you will notice a bump on your big toe joint. The big toe may turn in toward the second toe and the tissues surrounding the joint may be swollen and tender. Bunions can come from a variety of causes, including diabetes, rheumatoid arthritis, or foot mechanics that place too much load on the ball of your foot. If untreated, bunions can worsen, leading to other serious complications, and even potentially require surgery. Early treatment is best, so if you?re suffering from bunions it?s smart to see a podiatrist for proper treatment and care.
A bunion is an often painful enlargement of bone or tissue around the joint at the base of the big toe. If you have a bunion, you will notice a bump on your big toe joint. The big toe may turn in toward the second toe and the tissues surrounding the joint may be swollen and tender. Bunions can come from a variety of causes, including diabetes, rheumatoid arthritis, or foot mechanics that place too much load on the ball of your foot. If untreated, bunions can worsen, leading to other serious complications, and even potentially require surgery. Early treatment is best, so if you?re suffering from bunions it?s smart to see a podiatrist for proper treatment and care.
Causes
Long periods of pressure from a tight-fitting shoe can cause the inflammation and the pain. This often happens when the big toe is forced into a position where it presses inward and overlaps the second toe. The base of the big toe then is pushed beyond normal alignment of the foot, resulting in the prominence typical of a bunion.
Symptoms
Most patients complain of pain directly on the bunion area, within the big toe joint, and/or on the bottom of the foot. The bunion may become irritated, red, warm, swollen and/or callused. The pain may be dull and mild or severe and sharp. The size of the bunion doesn?t necessarily result in more pain. Pain is often made worse by shoes, especially shoes that crowd the toes. While some bunions may result in significant pain, other bunions may not be painful at all.
Diagnosis
Looking at the problem area on the foot is the best way to discover a bunion. If it has the shape characteristic of a bunion, this is the first hint of a problem. The doctor may also look at the shape of your leg, ankle, and foot while you are standing, and check the range of motion of your toe and joints by asking you to move your toes in different directions A closer examination with weight-bearing X-rays helps your doctor examine the actual bone structure at the joint and see how severe the problem is. A doctor may ask about the types of shoes you wear, sports or activities (e.g., ballet) you participate in, and whether or not you have had a recent injury. This information will help determine your treatment.
Non Surgical Treatment
Sometimes observation of the bunion is all that?s needed. To reduce the chance of damage to the joint, periodic evaluation and x-rays by your surgeon are advised. In many other cases, however, some type of treatment is needed. Early treatments are aimed at easing the pain of bunions, but they won?t reverse the deformity itself. These include changes in shoewear. Wearing the right kind of shoes is very important. Choose shoes that have a wide toe box and forgo those with pointed toes or high heels which may aggravate the condition. Padding. Pads placed over the area of the bunion can help minimize pain. These can be obtained from your surgeon or purchased at a drug store. Activity modifications. Avoid activity that causes bunion pain, including standing for long periods of time. Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation. Icing. Applying an ice pack several times a day helps reduce inflammation and pain. Injection therapy. Although rarely used in bunion treatment, injections of corticosteroids may be useful in treating the inflamed bursa (fluid-filled sac located around a joint) sometimes seen with bunions. Orthotic devices. In some cases, custom orthotic devices may be provided by the foot and ankle surgeon. 
Surgical Treatment
Surgery can be a very successful treatment for bunions and could be considered if you are having pain that is affecting your function on a regular basis, for instance, pain during sports or wearing work shoes. It is important, however, that you are seen by a consultant orthopaedic foot and ankle surgeon who has undergone specialist training with a foot and ankle fellowship. There are many different surgical techniques and it is important that your surgeon is expert in several of these so that you have the one that is best for your unique deformity. Bunion removal is usually done under general anesthesia. This means you will be asleep throughout the procedure. The operation can be performed as a day-case, but an overnight stay in hospital is sometimes required. Your surgeon will explain the benefits and risks of having bunion surgery, and will also discuss the alternatives treatments.
Prevention
The simplest way to reduce your chance of developing foot bunion or bunionette problems is to wear good-fitting shoes. Avoid high heels as they push your feet forwards to the front of the shoe where they get squashed. Also avoid narrow fitting shoes, especially those that are pointed at the front with a narrow toe box as again, these place pressure through the toes pushing them inwards. Shoes should be comfortable and leave enough room for you to wiggle your toes. Remember, bunions rarely affect non-shoe wearing people. Exercising your feet can also help. By strengthening the foot muscles you can improve your foot position which can help reduce foot bunion problems. Simple exercises like picking up small objects with your toes can help.
Do I Suffer From Over-Pronation Of The Foot
Over pronation of the foot is commonly referred to as "flat feet." Many middle-aged men and women suffer from over pronation over time and as a result of wearing poor-fitting shoes, continuing with repetitive exercising habits, or walking in high heels for long periods over several years. Regular speed-walkers often experience over pronation as well as a result of this activity.

Causes
Over-pronation is very prominent in people who have flexible, flat feet. The framework of the foot begins to collapse, causing the foot to flatten and adding additional stress to other parts of the foot. Therefore over-pronation can often lead to a case of Plantar Fasciitis, Heel Spurs, Metatarsalgia, Post-tib Tendonitis and/or Bunions. There are many causes of flat feet. Obesity, pregnancy or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. People with flat feet often do not experience discomfort immediately, and some never suffer from any discomfort at all. However, when symptoms develop and become painful, walking becomes awkward and causes increased strain on the feet and calves.
Symptoms
Not all foot injuries affecting runners are necessarily down to a particular running gait; it is rarely that simple to diagnose how a foot problem developed . Simply being an overpronator does not mean that a foot injury has been caused by the running gait and it could be due to a number of factors. However mild to severe overpronators tend to be at a higher risk of developing musculoskeletal problems due to the increased stresses and strains which are placed on the body when the foot does not move in an optimum manner. The following injuries are frequently due to overpronation of the feet. Tarsal tunnel syndrome. Shin splints. Anterior compartment syndrome. Plantar fasciitis. Achilles tendonitis. Bunions. Sesamoiditis. Stress fractures. Back and hip pain. Ankle pain.
Diagnosis
People who overpronate have flat feet or collapsed arches. You can tell whether you overpronate by wetting your feet and standing on a dry, flat surface. If your footprint looks complete, you probably overpronate. Another way to determine whether you have this condition is to simply look at your feet when you stand. If there is no arch on the innermost part of your sole, and it touches the floor, you likely overpronate. The only way to truly know for sure, however, is to be properly diagnosed by a foot and ankle specialist.

Non Surgical Treatment
Side Step with Opposite Reach. This exercise is designed to load the "bungee cord system" of the gluteal muscle and its opposite, latissimus dorsi muscle to keep the foot from overpronating. Because the opposite arm swings across the front leg when walking, this exercise creates tension in the muscles all the way from the front foot, across the back of the hips and back, to the fingers of the opposite hand. Movement Directions. Stand with left foot on top of the dome of the BT. (Note: For added balance, the right foot can tap on the ground, if needed). Reach right leg out to the side of the BT, and tap the ground while squatting down on the left side and reaching right arm across the left knee. Push down with left big toe while squatting. This activates the arch of the left foot and strengthens all the stabilizing muscles on the left side of the lower body. Return to starting position. Perform 8 to 10 repetitions on each leg.
Surgical Treatment
Calcaneal "Slide" (Sliding Calcaneal Osteotomy) A wedge is cut into the heel bone (calcaneus) and a fixation device (screws, plate) is used to hold the bone in its new position. This is an aggressive option with a prolonged period of non-weightbearing, long recovery times and many potential complications. However, it can and has provided for successful patient outcomes.
What Exactly Is Severs Disease?
Sever?s disease occurs in children when the growing part of the heel is injured. This growing part is called the growth plate. The foot is one of the first body parts to grow to full size. This usually occurs in early puberty. During this time, bones often grow faster than muscles and tendons. As a result, muscles and tendons become ?tight.? The heel area is less flexible. During weight-bearing activity (activity performed while standing), the tight heel tendons may put too much pressure at the back of the heel (where the Achilles tendon attaches). This may injure the heel.
Causes
Apart from age, other factors that may contribute to developing Sever?s disease include physical activity, any form of exercise that is weight bearing through the legs or stresses the soft tissue can exacerbate the pain of the disease. External factors, for example, running on hard surfaces or wearing inappropriate shoes during sport. Overuse injury, very active children may repeatedly but subtly injure the bones, muscles and tendons of their feet and ankles. In time, the accumulated injuries cause symptoms.
Symptoms
Patients with Severs disease typically experience pain that develops gradually in the back of the heel or Achilles region. In less severe cases, patients may only experience an ache or stiffness in the heel that increases with rest (especially at night or first thing in the morning). This typically occurs following activities which require strong or repetitive contraction of the calf muscles, such as running (especially uphill) or during sports involving running, jumping or hopping. The pain associated with this condition may also warm up with activity in the initial stages of the condition. As the condition progresses, patients may experience symptoms that increase during activity and affect performance. Pain may also increase when performing a calf stretch or heel raise (i.e. rising up onto tip toes). In severe cases, patients may walk with a limp, have difficulty putting their heel down, or be unable to weight bear on the affected leg. Pain may also increase on firmly touching the affected region and occasionally a bony lump may be palpable or visible at the back of the heel. This condition typically presents gradually overtime and can affect either one or both lower limbs.
Diagnosis
Sever condition is diagnosed by detecting the characteristic symptoms and signs above in the older children, particularly boys between 8 and 15 years of age. Sometimes X-ray testing can be helpful as it can occasionally demonstrate irregularity of the calcaneus bone at the point where the Achilles tendon attaches.
Non Surgical Treatment
Sever?s disease is a self-limiting problem, because as your child grows the growth plate will eventually fuse with the main body of the heel bone. This happens at about 14 -15 years of age. Once foot growth is complete and the growth plate has fused, the symptoms will resolve. In the meantime, treatment by your Podiatrist will help your child return to normal sporting activities without heel pain slowing him/her down.
Recovery
This condition is self limiting - it will go away when the two parts of bony growth join together - this is natural. Unfortunately, Sever's disease can be very painful and limit sport activity of the child while waiting for it to go away, so treatment is often advised to help relieve it. In a few cases of Sever's disease, the treatment is not successful and these children will be restricted in their activity levels until the two growth areas join - usually around the age of 16 years. There are no known long term complications associated with Sever's disease.
Achilles Tendon Rupture Rehabilitation
Overview
 A total rupture of the achilles tendon is a complete tear of the tendon and typically affects men over the age of 40 involved in recreational sport. A complete rupture of the achilles tendon is not always recognized at the time of injury, however it is very important it is treated properly as soon as possible to increase the chances of a good recovery.
A total rupture of the achilles tendon is a complete tear of the tendon and typically affects men over the age of 40 involved in recreational sport. A complete rupture of the achilles tendon is not always recognized at the time of injury, however it is very important it is treated properly as soon as possible to increase the chances of a good recovery.
Causes
The Achilles tendon is most commonly injured by sudden plantarflexion or dorsiflexion of the ankle, or by forced dorsiflexion of the ankle outside its normal range of motion. Other mechanisms by which the Achilles can be torn involve sudden direct trauma to the tendon, or sudden activation of the Achilles after atrophy from prolonged periods of inactivity. Some other common tears can occur from overuse while participating in intense sports. Twisting or jerking motions can also contribute to injury. Fluoroquinolone antibiotics, famously ciprofloxacin, are known to increase the risk of tendon rupture, particularly achilles.
Symptoms
A classic sign of an Achilles tendon rupture is the feeling of being hit in the Achilles are. There is often a "pop" sound. There may be little pain, but the person can not lift up onto his toes while weight bearing.
Diagnosis
Laboratory studies usually are not necessary in evaluating and diagnosing an Achilles tendon rupture or injury, although evaluation may help to rule out some of the other possibilities in the differential diagnosis. Plain radiography. Radiographs are more useful for ruling out other injuries than for ruling in Achilles tendon ruptures. Ultrasonography of the leg and thigh can help to evaluate the possibility of deep venous thrombosis and also can be used to rule out a Baker cyst, in experienced hands, ultrasonography can identify a ruptured Achilles tendon or the signs of tendinosis. Magnetic resonance imaging (MRI). MRI can facilitate definitive diagnosis of a disrupted tendon and can be used to distinguish between paratenonitis, tendinosis, and bursitis.
Non Surgical Treatment
Treatment of the initial injury is with use of ice, elevation, and immobilization. If suspected you should contact your podiatrist or physician. Further treatment with continued immobilization, pain medication, or anti-inflammatory medications may be advised. If casted the foot is usually placed in a plantarflexed position to decrease the stretch on the tendon. As healing progresses the cast is changed to a more dorsiflexed position at the ankle. The casting processes can be up to 8 weeks or more. 
Surgical Treatment
The goal of surgery is to realign the two ends of the ruptured tendon to allow healing. There are multiple techniques to accomplish this goal that will vary from surgeon to surgeon. Recovery from this injury is usually very successful with return to full function in approximately 6 months. Post operatively casting is required with the use of crutches or other means to remain non-weightbearing for 4-8 weeks. This is followed by a course of physical therapy. Partial rupture may or may not require surgical intervention depending on the extent of injury but cast immobilization is a common requirement.
Prevention
Achilles tendon rupture can be prevented by avoiding chronic injury to the Achilles tendon (i.e. tendonitis), as well as being careful to warm up and stretch properly before physical activity. Additionally, be sure to use properly fitting equipment (e.g. running shoes) and correct training techniques to avoid this problem!